Overview:
- The report identifies five core social determinants: financial resources, health care, food and nutrition, safety, and social support.
- The report shows how these dynamics interact to shape health outcomes.
- Scroll to the bottom for tips on civic action you can take around this issue.
A new analysis from the Citizens Research Council of Michigan finds that Michigan is faring worse than the national average on almost every major health metric, with widening disparities by race, income, and education.
The report argues that improving residents’ financial stability is the most powerful way to reverse declining health trends.
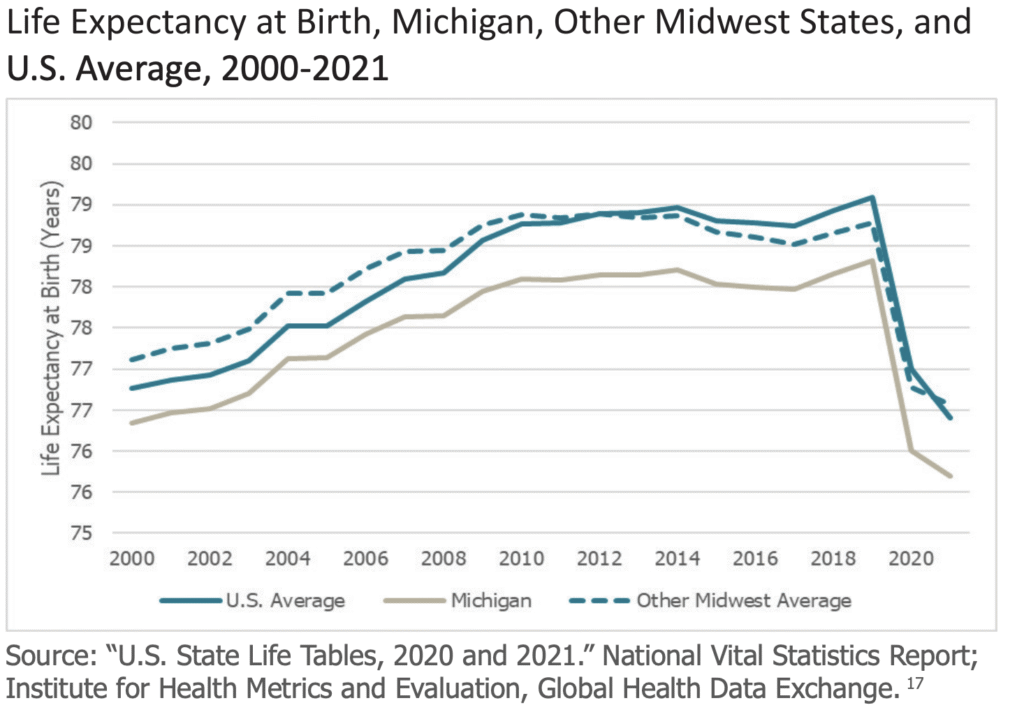
The Tuesday report, Social Determinants of Health: Pathways to a Healthier Michigan, concludes that Michigan residents experience lower life expectancy, higher premature death rates, and poorer self-reported health than people in other Midwestern states and peer nations. These outcomes are especially severe for Black Michiganders.
“The centrality of financial resources – education, employment, and income – is the story of Michigan’s lagging health outcomes,” Eric Lupher, Citizens Research Council president, said in a statement.
Among the report’s findings:
- Michigan ranks below the national average and its Midwestern peers across most major health outcomes, including life expectancy, premature death, self-reported health status, and chronic disease rates.
- Racial and economic disparities in Michigan are wider than national averages, with Black residents experiencing significantly worse outcomes across multiple indicators.
- Financial resources — education, income, and employment — are the most influential drivers of health outcomes and a common thread linking disparities across the state.
- Access to health care in Michigan is better than in many states. Still, the U.S. system as a whole underperforms compared with other developed countries, limiting the state’s ability to close gaps without broader reforms.
- Food access, neighborhood safety, and social support systems vary widely across the state, contributing to uneven health risks, especially for low-income and rural communities.
- The report emphasizes that “all policy is health policy,” highlighting the need for cross-sector strategies, from housing and transportation to education and economic development, to improve population health meaningfully.
This aligns with Planet Detroit’s earlier reporting in Detroit, which noted that access to clinical care accounts for just 20% of the variation in health outcomes. Much more critical to our health is our environment, socio-economic status, education, neighborhood and housing, where and how we work, and the family and friends that make up our social support networks.
Michigan’s economic, educational challenges deepen health inequities
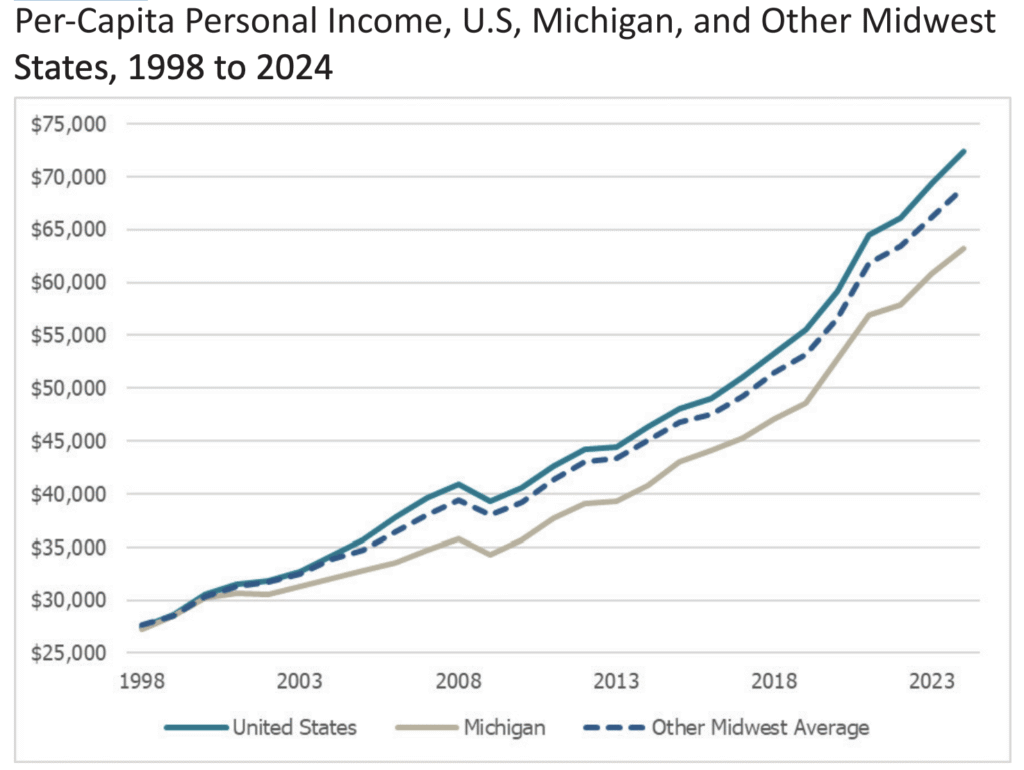
These findings align with broader statewide trends documented in the recent Michigan in a New Era report, which shows that the same structural drivers affecting education and income are also influencing health outcomes:
- Michigan ranks 35th in real median household income and 50th in income growth over the past 25 years, limiting families’ ability to afford healthy food, stable housing and quality care.
- The state has seen a long decline in educational performance, falling from 16th to 44th in fourth-grade reading and 10th to 34th in math over two decades. Education is a core determinant of income and long-term health.
- One in four Michigan students is chronically absent, among the highest rates nationally — a key predictor of lower graduation rates, lower earnings, and worse adult health.
- The report describes decades of industrial disruption, talent outmigration, and policy inconsistency, weakening economic mobility and community stability.
Together, these conditions reflect what both reports emphasize: Michigan’s health challenges cannot be separated from its long-standing economic and educational struggles.
Financial resources key to health outcomes
Karley Abramson, the study’s author and a CRC researcher who studies health, environment, and economic disparities, said the concerns raised in the study align with broader statewide patterns. For example, she said financial resources consistently determine who can avoid exposure to pollution and who cannot.
“What we learned from analyzing all the pieces of data is that financial resources are at the root of so many pathways toward better health outcomes,” Abramson said. “If you’re living in an environment that has higher pollution, really the only way out of that is to afford your way out.”
The pattern holds both statewide and within Michigan’s counties, she said. “When you trace it back again and again, it comes back to financial resources,” she said.
“It’s significant that this is the very area where Michigan struggles, because it’s so central to health outcomes. It shows why we need to zoom out from narrow conversations about health care alone when we talk about policy.”
Health disparities across Metro Detroit
Geographic disparities in the region are stark. For example, the highest average life expectancy in the region is among the white population in Oakland County at 80.1 years. The lowest is among the Black population in Macomb County at 69.7 years.
The CRC report identifies five key “fundamental resources” that shape health outcomes: financial resources, health care, food and nutrition, safety, and social support. It emphasizes that financial resources such as education, employment and income are the central driver linking the others.
“In every area of public policy, there is a nexus to health,” the report states.
One potential solution is community health workers. Planet Detroit’s reporting earlier this year on community health workers revealed how health systems are turning to working with advocates with lived experience to mitigate health risks driven by economic threats.
These stories demonstrate how community health workers help people navigate housing, food access, and chronic illness — underlining the connection between financial instability, social supports, and health outcomes.
Below-average air quality, violence stress health
While Michigan performs slightly better than the national average on measures such as insurance coverage and health care availability, the report finds the state still lags behind international counterparts and faces structural challenges in cost, access and provider shortages. It also highlights above-average levels of community violence and below-average air quality as additional stressors on health.
The authors argue that policymakers should treat population health as a core economic and civic priority, noting that poor health undermines workforce participation, increases health-care spending and slows progress on other state goals.
They call for long-term investments in education, income growth and reducing racial and economic disparities as the most effective strategies to improve health outcomes.
How residents can use this information in upcoming decisions
Abramson said Michigan residents can use the findings to better evaluate candidates, policies, and budget decisions that directly affect health outcomes. Since financial resources are the strongest driver of health, voters should look for policymakers who prioritize raising incomes, improving education, expanding employment opportunities, and addressing racial disparities, she saiud.
“When Michigan residents are engaging with the political process and thinking about what they want our legislators to focus on, try to pick the ones that are focusing on policies that you think would help achieve this goal,” Abramson said.
No single political ideology is tied to improving financial stability, she said. Approaches might include economic development strategies, job creation, or cash-assistance programs — but residents should look for clear, concrete proposals that expand financial resources for low- and moderate-income households.
While many candidates say they support improving education, income, and employment, residents should ask more specific questions about how those policies will be carried out, Ambramson said.
“Asking and trying to get people to focus more specifically with policies is what residents should be looking out for when they are engaging and making those decisions.”
🗳️ What’s next? Tips for civic action
Why it matters
📉 Michigan’s health outcomes lag behind national and Midwestern averages, with especially wide racial and income-based gaps. The CRC report finds that financial resources, education, housing, safety, and social support all shape who gets sick and who stays healthy.
Who’s making civic decisions
🏛️ State lawmakers, the governor’s office, and state agencies such as the Michigan Department of Health and Human Services (MDHHS); Environment, Great Lakes, and Energy; and the Department of Education all influence policies that affect income, housing, food access, health care, and safety. Local governments, school boards, health systems, and employers also make decisions that shape social determinants of health where you live.
How to take civic action now
- 🏛️ Ask your state lawmakers how they are addressing the social determinants of health in budget and policy decisions — including income supports, housing, transportation, education, and public health funding.
- 🏥 Contact your local health department or hospital system and ask how they are incorporating social determinants of health into their community health plans and investments.
- 🧮 Use the report in your advocacy by citing its findings when submitting public comments, testifying at hearings, or meeting with local officials about housing, income, transportation, safety, or education.
- 🤝 Join or support community groups working on issues like affordable housing, food access, environmental quality, and economic opportunity in your neighborhood.
What to watch for next
🗓️ Watch upcoming state and local budget cycles, legislation, and agency plans that relate to income, education, housing, transportation, health care access, and safety. The report stresses that “all policy is health policy,” so debates in these areas are also debates about health.
Civic impact
🌍 When residents use evidence from reports like this one to ask questions, attend meetings, and submit comments, they help push decision-makers to consider health impacts and reduce disparities across Michigan.
Planet Detroit’s Reporting on Social Determinants of Health and Community Health Workers
How to understand and connect with community health workers in Michigan
Community Health Workers in Michigan are vital in bridging healthcare gaps, offering essential support like food, housing, and insurance enrollment. Certified and trained, they build trust and provide care to underserved communities, especially amid federal Medicaid cuts threatening their funding.
More than medicine: How a community health worker keeps one patient housed – and alive
Community health workers at Trinity Health Michigan are tackling food insecurity and housing challenges, offering support with Medicaid and utility shutoffs, while empowering residents through the hospital’s urban farm and food hub.
How a phone call a week helped one Detroiter manage diabetes — and avoid the ER
Read our entire series on Community Health Workers here>>> When Terry Pita’s doctor told her she needed to start insulin, she burst into tears. “I just didn’t want to take shots,” she said. “I still cringe.” Pita, who has managed Type 2 diabetes for more than a decade, had struggled for years to bring her…
As Medicaid cuts loom, are Michigan’s community health workers in jeopardy?
Michigan’s Medicaid reimbursement for certified Community Health Workers marks a pivotal moment in health equity and access, yet looming federal budget cuts threaten to unravel these advances, impacting economic stability for vulnerable communities.