Overview:
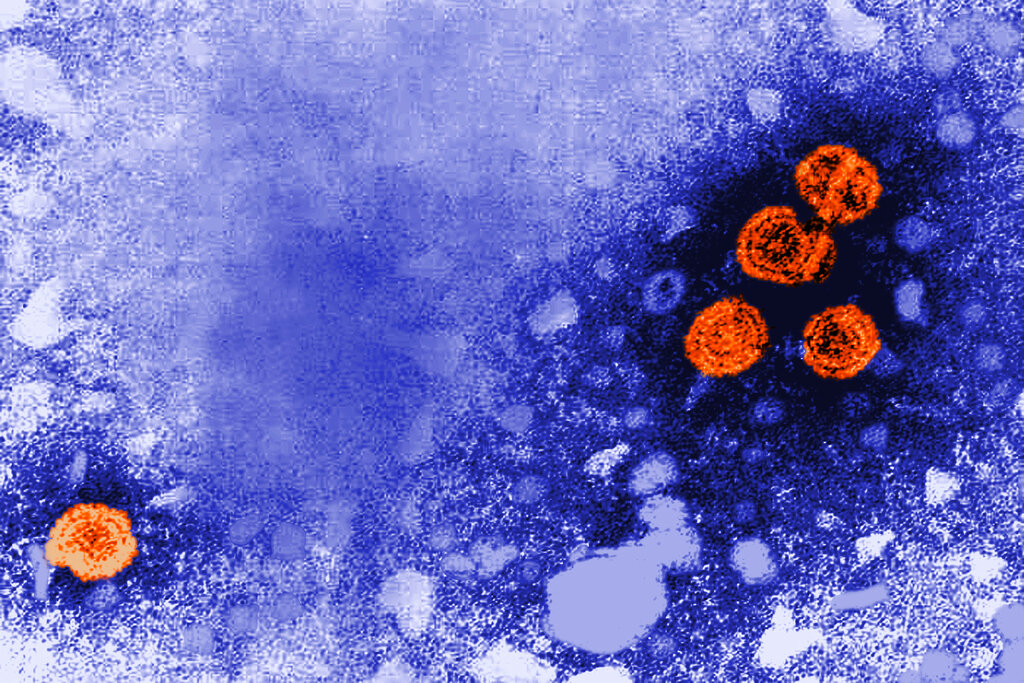
- The Advisory Committee on Immunization Practices voted to shift from universal newborn hepatitis B vaccination to a screening-based approach, a move Michigan health officials oppose.
-Despite five years of zero perinatal transmission, vaccine rates are dropping in Michigan.
- Michigan's hepatitis B incidence is 40% above the national average, with significant racial disparities.
A federal vaccine advisory committee voted last week to roll back the longstanding recommendation that all newborns receive the hepatitis B vaccine within 24 hours of birth — a decision Michigan health officials rejected.
The Advisory Committee on Immunization Practices, overhauled earlier this year by Health and Human Services Secretary Robert F. Kennedy Jr., voted Dec. 5 to shift the country from universal newborn vaccination to a screening-based approach.
Under the new recommendation, parents of babies born to mothers who test negative for hepatitis B would engage in “shared clinical decision-making” with their doctor about whether to vaccinate at birth.
The vote effectively returns the country to a policy framework abandoned in 1991, after risk-based screening repeatedly failed to identify infected mothers and stop transmission to their babies.
In a statement, Michigan’s Department of Health and Human Services said it “strongly disagrees” with the decision and urged families and providers to continue following immunization schedules from the American Academy of Pediatrics and the American Academy of Family Physicians.
The state’s own data underscores what’s at stake: Michigan has recorded zero cases of perinatal hepatitis B transmission for five consecutive years, from 2021 through 2025. In 2023, 89 babies were born to mothers who tested positive, and every one was protected.
But that success may already be eroding. State data show that 75.2% of Michigan toddlers born between late 2022 and early 2024 received the birth dose within three days of life. For babies born in the first half of 2025, that number dropped to 68.9% — a decline that began before the ACIP vote and could accelerate now.
Hepatitis B in Michigan
The state has particular reason for concern. Michigan’s chronic hepatitis B incidence rate is approximately 40% higher than the national average, according to state surveillance data.
Racial disparities are stark: Asian Michiganders are diagnosed at more than six times the statewide rate, and Black Michiganders at more than four times the rate of white residents.
White Michiganders are far from immune: they account for 49% of the state’s acute hepatitis B cases.
The virus doesn’t discriminate by zip code or demographic profile, which is why federal officials moved to universal vaccination three decades ago. Studies found that 35% to 65% of mothers who tested positive for hepatitis B had no identifiable risk factors and would have been missed under a screening-based approach.
Black and Asian Michiganders are hospitalized for hepatitis B at rates five to six times higher than white residents. Nationally, Black Americans are diagnosed at four times the rate of white Americans and are more than twice as likely to die from the disease.
A 32-year view from the clinic
Dr. Kimberly Brown, the associate medical director of the Henry Ford Transplant Institute, has spent 32 years treating patients with liver disease and is the hospital’s former chief of gastroenterology and hepatology.

“When I first started practicing, hepatitis B was a much more common disease to transplant,” Brown said.
“It has now become much, much less common, and I think it’s really a direct result of fewer people developing the chronic infection.”
The timing of vaccination matters enormously. If a baby acquires hepatitis B at birth, there’s a 90% chance of developing chronic infection, Brown said. Adults who contract the virus have only a 4% to 5% chance of becoming chronically infected.
“Vaccination at a very early age is really important, because that’s when our immune system is least likely to be able to fight off the infection,” she said.
An estimated 25% of chronically infected patients will eventually die of their disease. Many arrive at Brown’s clinic already in crisis.
“Many, many patients come to me after being diagnosed, and they already have cirrhosis of the liver,” Brown said. “It’s a disease that’s been going on for many, many years, but yet it’s only recognized when they develop a complication.”
The limits of screening
The new recommendation assumes that if a mother tests negative during pregnancy, her baby faces no immediate risk. Brown is skeptical.
“The recommendations to test mothers has been in place since 1988, and still today, after all these many years, as many as 18% of women are not tested,” she said. “If you’re not tested, then you don’t know which infants are at risk.”
About half of people with hepatitis B don’t know they’re infected, she said — including some who received the vaccine as adults, unaware they were already carrying the virus.
A lifelong disease with mounting costs
For infants who acquire hepatitis B, the consequences unfold over decades. The virus attacks the liver silently. By the time symptoms appear, patients may already have cirrhosis or cancer.
There is no cure. Treatment with antiviral medications can suppress the virus, but most patients require lifelong therapy. As the disease progresses, costs compound: regular monitoring for liver cancer, managing complications like internal bleeding and fluid buildup, and treating liver failure.
“Patients who have cirrhosis are then at risk of liver failure,” Brown said. “The cost, as patients progress, becomes increasingly high.”
What parents should know
Despite the ACIP vote, the hepatitis B vaccine remains available to any parent who wants it. Insurance will continue to cover it. The American Academy of Pediatrics, the American Academy of Family Physicians, and Michigan’s health department all continue to recommend it.
Brown said she would tell any parent in metro Detroit the same thing.
“I would support vaccination at birth,” she said. “It protects infants from acquiring the disease and then facing all those long-term complications.”
In the liver disease field, Brown said, the hepatitis B vaccine is known as “the only vaccine against cancer.”
“I worry for patients because, if they are exposed and acquire the infection and become chronically infected, they’re looking at a lifetime of disease that we could have prevented,” she said.
“And there’s also a risk to the rest of us, because those are the individuals that can transmit the infection to other people.”
Editor’s note: This story has been updated to correct Dr. Kimberly Brown’s title. She is the associate medical director of the Henry Ford Transplant Institute and is the hospital’s former chief of gastroenterology and hepatology.
MORE PUBLIC HEALTH NEWS
Michigan’s health is falling behind, new report warns — and financial insecurity is to blame
Michigan performs worse than national and Midwestern averages across most major health indicators and faces especially wide racial and economic disparities.
Detroit’s urban farms, food aid groups rally to close SNAP gap: ‘Perfect storm of hungry people’
Among some of the city’s urban farms, the SNAP pause spotlights a broader mission to make Detroit a food sovereign city, capable of feeding residents healthy and culturally relevant food all year long.
Wyandotte officials vote against restoring fluoride to drinking water: ‘I have my reasons why’
Wyandotte drinking water has not been treated with fluoride in a decade, which the state flagged in an April report that found “significant deficiencies” in the city’s drinking water system.